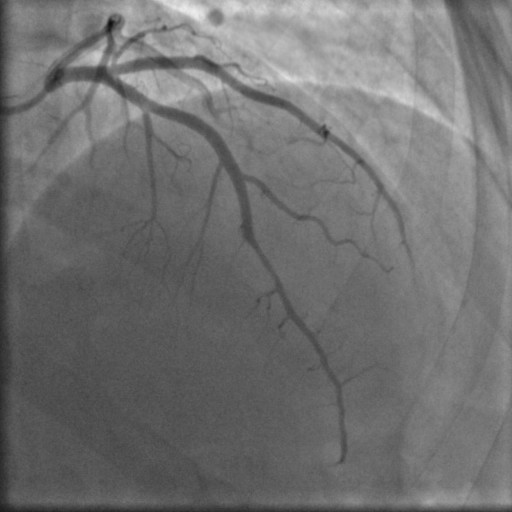
A 41-year-old woman went to ED referring two episodes of oppressive chest pain radiating to the jaw and left arm occurring at rest in the past 24 hours, lasting 5-20 minutes. She was a smoker with no other cardiovascular risk factor. The ECG on admission showed no signs of acute ischemia, while TTE showed apical hypokinesia with LVEF 60% and serial troponin I levels were elevated (0.3-0.4 ng/ml). A diagnosis of NSTEMI was made and the patient underwent coronary angiography, which revealed a calibre reduction of <50% in the mid-distal LAD, consistent with an intramural hematoma,with TIMI 3 distal flow; no significant stenosis in CX and RCA. Given her stable clinical status and absence of high-risk features, a conservative treatment strategy was adopted. CMR showed normal biventricular ejection fraction, subtle edema in the apical septum and a subepicardial enhancement stria in the mid-basal inferior wall. Discussion: Spontaneous coronary artery dissection is a non-atherosclerotic cause of acute coronary syndrome, rare in general population but not infrequent among young women, reaching 35% of all cases of AMI in women under 50. SCAD is characterized by a non-traumatic separation of the coronary wall due to the formation of an intramural hematoma, which can compress the vascular lumen, leading to myocardial ischemia, indistinguishable from atherosclerotic ACS by symptoms and sings. Being distinct from atherosclerotic ACS in pathophysiology, SCAD requires a different and tailored approach. Despite this, significant gaps remain in evidence-based guidelines for SCAD management due to a lack of prospective studies. Current strategies are based on expert opinions from observational data, suggesting conservative strategy in most patients. Revascularization is reserved for ongoing ischemia, left main dissection, hemodynamic or electrical instability, though PCI is often unsuccessful and carries significant risk of dissection’s propagation. Conservative approach leads to spontaneous lesion healing in majority of cases. Pharmacologic therapy focuses on beta-blockers to reduce arterial wall sheer stress and individualized use of antiplatelet therapy. For conservatively managed patients, SAPT over DAPT is usually recommended, but no specific study has been carried out to evaluate the efficacy of antiplatelet therapy in SCAD. For now, we are treating a condition with a hemorrhagic primum movens using evidences derived from studies on patients with a thrombotic disease.