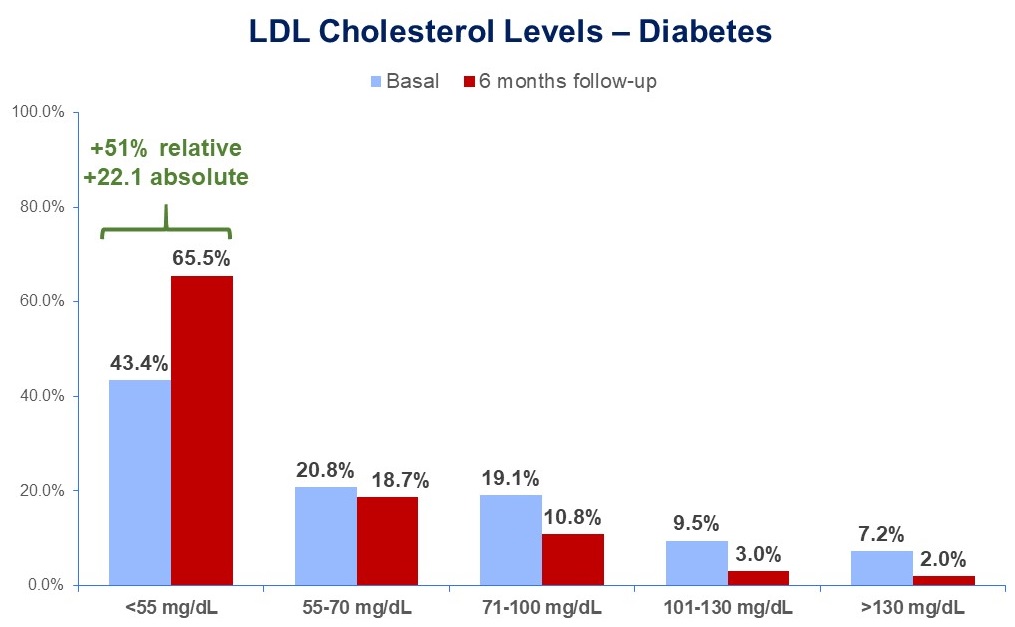
Background. Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in people with diabetes, making secondary prevention strategies critical to improving patient outcomes. Purpose. To try to narrow the gap between what is recommended by the current guidelines and what is implemented in clinical practice in diabetic patients, we designed a national implementation science project, named BRING-UP Prevention, based on educational programmes and patient data collection. Methods. BRING-UP Prevention is a nationwide, observational, prospective, multicentre study enrolling patients with a documented prior atherothrombotic event in 2 enrolment phases preceded by an educational intervention to discuss guideline recommendations. Primary endpoint: Rate of patients achieving target LDL cholesterol (<55 mg/dL). Secondary endpoints: rate of patients achieving target blood pressure (<130/80 mmHg), rate of diabetic patients achieving target HbA1c (<7%), rate of overweight patients (BMI >27 kg/m2) achieving at least 10% weight loss. The first phase has recently been completed. Results. Over 3 months, 189 cardiology centres collected data on 4790 patients, of whom 1317 (27.5%) had diabetes. Follow-up data were available for 1229/1317 patients (93.3%). The figure shows LDL cholesterol levels at baseline and after 6 months. The rate of diabetic patients with LDL cholesterol <55 mg/dL increased from 43.4% to 65.5% with treatment mainly based on high-intensity statins in association with ezetimibe (65.8% of patients). PCSK9 inhibitors were used in 5.6% of patients. HbA1c, measured at follow-up in only 61.8% of patients, was <7% in only 46.7% of patients. Pts with blood pressure <130/80 mmHg were 36.5% at baseline and 42.5% at follow-up. The rate of pts doing light physical activity increased from 36.2% to 50.1%. At baseline, 46.1% of patients had a BMI >27, which decreased to 43.3% at follow-up. 11.3% of overweight patients lost more than 10% of their body weight during follow-up. The most commonly prescribed antidiabetic medications at both baseline and follow-up were metformin (51.1%), SGLT2 inhibitors (49.6%), insulin (27.1%), and GLP-1 RA (19.4%). Conclusions. This study shows that it is possible to improve adherence to the LDL cholesterol goal recommended by current guidelines with cost-effective drugs. There appears to be a need for more intensive strategies to improve blood pressure, HbA1c levels and lifestyle changes.