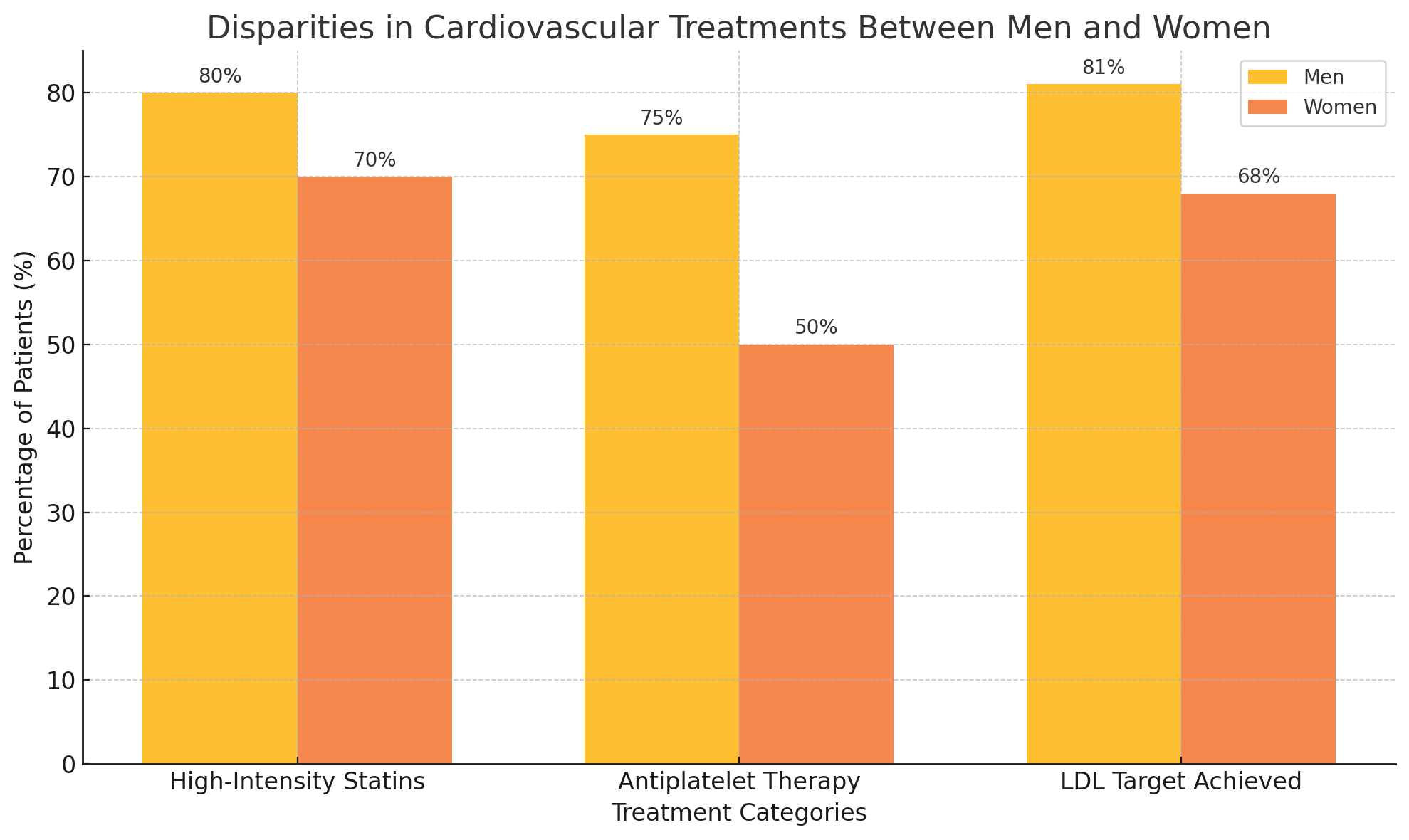
Cardiovascular diseases (CVDs) remain the leading cause of mortality worldwide, driven largely by modifiable risk factors. However, the impact and management of these risk factors vary significantly between men and women, often to the detriment of female patients. This systematic review explores these disparities, with a focus on innovative approaches to improve risk stratification and outcomes. Women present unique challenges in cardiovascular prevention. Adverse pregnancy outcomes (APOs)—including preeclampsia, gestational diabetes, and preterm delivery—are associated with a 3- to 7-fold increased risk of CVD later in life. Despite this, fewer than 20% of women with APOs receive targeted cardiovascular follow-up. Hypertension, often more prevalent and severe in postmenopausal women, is less likely to be adequately controlled, with blood pressure targets achieved in only 65% of women compared to 78% of men. Similarly, lipid management reveals striking gaps: only 68% of women at high cardiovascular risk reach LDL-C goals compared to 81% of men, with women more frequently prescribed low-potency statins. Diagnostic and therapeutic biases exacerbate these disparities. For example, women with acute coronary syndromes face a 50% higher likelihood of misdiagnosis, while non-obstructive coronary artery disease—a condition more common in women—remains underdiagnosed and undertreated. Even among those diagnosed, adherence to preventive therapies, such as statins and antiplatelet agents, is 20% lower in women than men, further widening the risk gap. Recent innovations provide hope for closing these gaps. High-sensitivity troponin assays, when paired with gender-specific thresholds, improve diagnostic accuracy in women by 5-fold. Machine learning algorithms incorporating sex-specific risk factors demonstrate a 15% improvement in predicting major adverse cardiovascular events in women. These tools underscore the importance of integrating gender-sensitive data into routine care. This review highlights the urgent need to reframe cardiovascular prevention with a gender-specific lens. By prioritizing the unique risk profiles and needs of women, we can not only reduce disparities but also pave the way for truly equitable cardiovascular care.