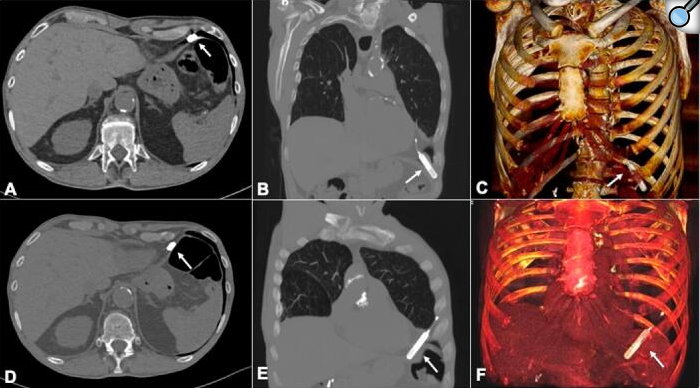
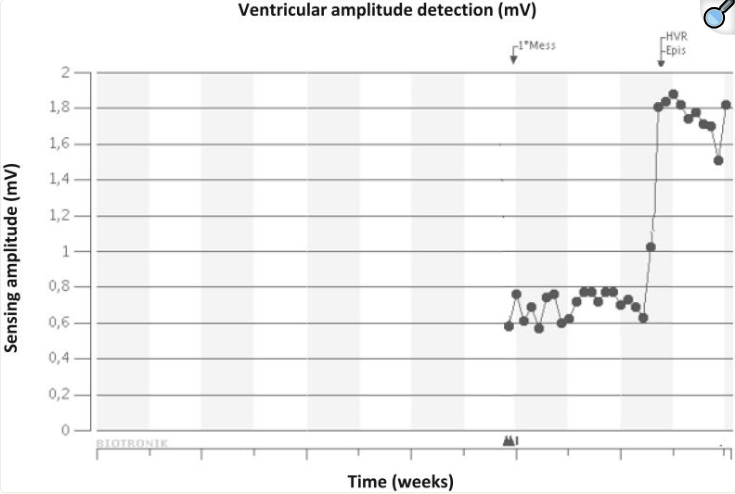
Introduction: Remote monitoring is recommended as part of the standard follow-up management strategy of ILRs. We report a case of asymptomatic ILR migration into the pleural cavity, unmasked by remote monitoring, and its multidisciplinary management. Case presentation: A 75-year-old man with paroxysmal AF was referred to our syncope unit for the evaluation of recurrent episodes of orthostatic T-LOC without prodromes. The result of the comprehensive cardiological evaluation was negative. An ILR with a long-sensing vector was implanted in the left anterior chest wall. At implantation, the measured R-wave amplitude was 0.4 mV. The patient was remotely monitored with the Biotronik Home Monitoring® system. Approximately 1 month later, an unstable R-wave amplitude varying from very high (>1.9 mV) to very low (<0.2 mV) values was recorded at remote monitoring. The patient's device was interrogated in the pacemaker clinic. It was not possible to achieve telemetric connection to the ILR at the implantation site. The only area where the ILR could be interrogated was the left posterior axillary site. Chest X-ray and CT scan confirmed migration of the ILR into the anterior costophrenic recess. The ILR was removed by uniportal VATS. Discussion: ILR migration into the pleural cavity is rare. It may be caused by an intraoperative technical mistake. If an excessive angle of penetration (>40°) is applied, the pocket tool might be inadvertently inserted through the intercostal space into the pleural cavity. Moreover, if the tip of the device was initially implanted deeply with angulation toward the intercostal muscle, the thin chest wall structure and the negative pressure of the pleural cavity could result in intrathoracic migration. From the analyses of the previous published cases the suspicion of ILR dislocation was suggested by patients' symptomatology or by the impossibility to telemetrically interrogate the ILR at routine clinical visit. In our case, the sudden and unexpected unstable R-wave amplitude flotation with very high values detected at device remote monitoring led us to evaluate the patient before the scheduled in-hospital clinical visit and to detect the ILR migration. Conclusion: ILR migration into pleural cavity is a rare complication of ILR implantation. ILR remote monitoring may be useful to early detect the sudden and unexpected R-wave amplitude flotation which may lead to ILR migration diagnosis.