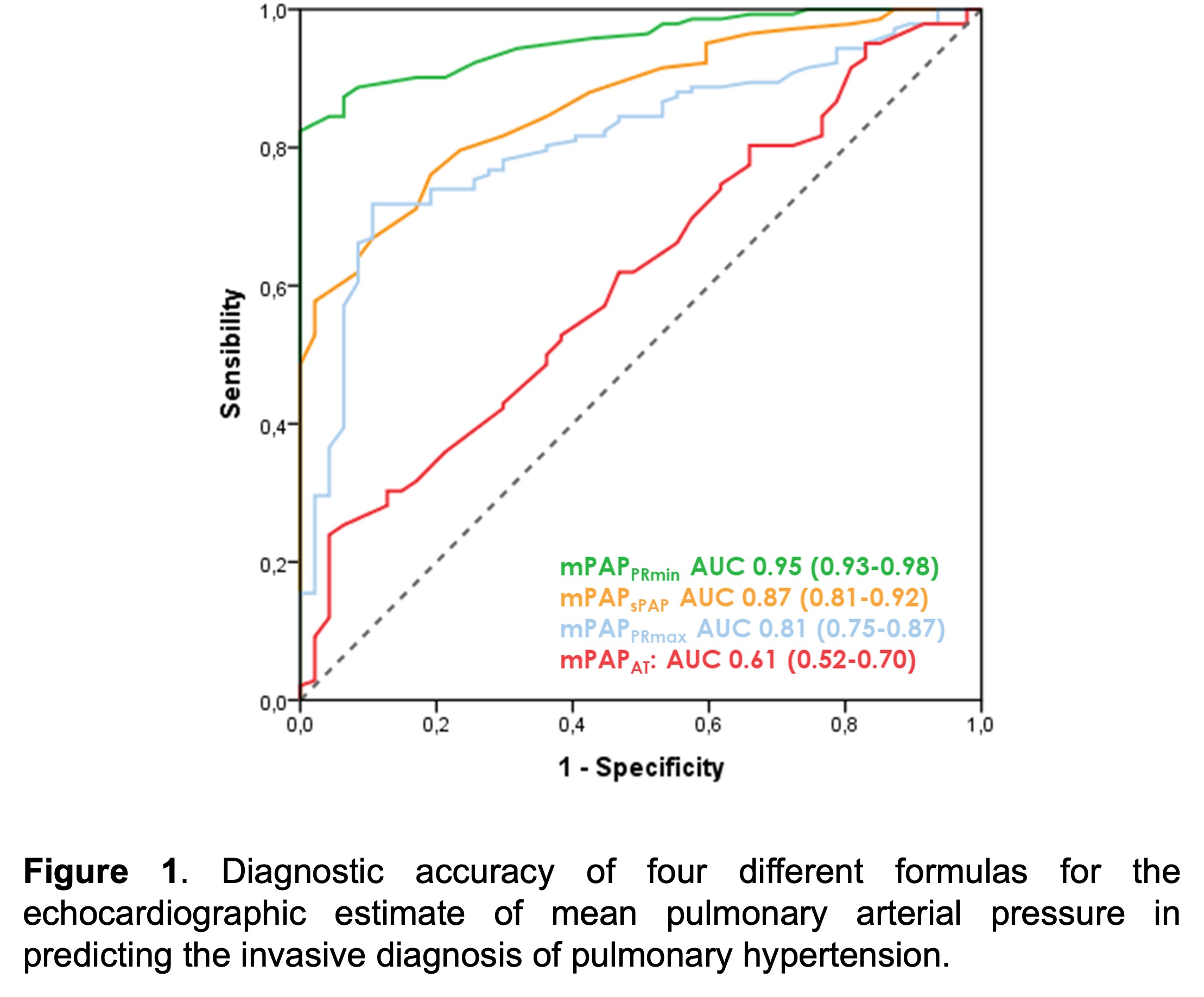
Background: Pulmonary hypertension (PH) is defined as an increase in mean pulmonary arterial pressure (mPAP) >20 mmHg at rest, as assessed by right heart catheterization (RHC). Echocardiography often serves as the first-line diagnostic examination for patients with suspected PH. However, no echocardiographic estimate of mPAP is currently recommended by guidelines, as the various formulas proposed to date lack large-scale diagnostic and prognostic validation. The aim of this study was to evaluate the diagnostic performance of different formulas for assessing mPAP through echocardiography in a large cohort of patients undergoing RHC for suspected PH. Methods and results: This study included 419 patients (216 men, aged 69±12 years) undergoing RHC for suspected PH. At RHC, mPAP was 28±8 mmHg, and according to the 2022 European Society of Cardiology guidelines, 313 patients (74.5%) were diagnosed with PH: 137 (33%) pre-capillary, 99 (24%) post-capillary, 95 (26%) combined, and 18 (4%) unclassified. Echocardiography was performed within 1.8±2.2 days of RHC and mPAP was estimated through four different formulas where applicable: 1)mPAPsPAP= 0.61*sPAP+2, where sPAP is systolic pulmonary arterial pressure (available in 419 patients [100%], mean value 32±9 mmHg); 2)mPAPAT= 80−(0.5*RVOT-AT), where RVOT-AT is the acceleration time of blood flow through right ventricular outflow tract (available in 351 patients [83%], mean value 32±16 mmHg); 3)mPAPPRmax= 4*(PRmax)2+RAP, where PRmax is the early-diastolic flow velocity of pulmonary regurgitation and RAP is the echocardiography estimate of right atrial pressure (available in 206 patients [49%], mean value 30±13 mmHg); 4)mPAPPRmin= 2/3*dPAP+1/3*sPAP, where dPAP= 4*(PRmin)2+RAP and PRmin is the end-diastolic flow velocity of pulmonary regurgitation (available in 419 patients [100%], mean value 28±8 mmHg). Each measure was correlated with invasive mPAP (ρ=0.86 for mPAPsPAP; ρ=0.28 for mPAPAT; ρ=0.70 for mPAPPRmax; ρ=0.93 for mPAPPRmin; all p<0.001). At receiver-operating characteristic (ROC) curve analysis (Figure 1), mPAPPRmin exhibited a substantially higher area under the curve (AUC 0.95, 95%CI 0.93-0.98) in identifying patients with PH compared to mPAPsPAP (AUC 0.87, 95%CI 0.81-0.92), mPAPPRmax (AUC 0.81, 95%CI 0.75-0.88) and mPAPAT (AUC 0.61, 95%CI 0.52-0.70). Conclusion: The echocardiographic estimate of mPAP, particularly when derived using the mPAPPRminformula, is feasible and highly accurate for diagnosing PH.